This article was medically reviewed by Dr. Najah Doka.
People who engage in high-risk personal behaviors or are in certain lines of work can be exposed to other people’s blood or bodily fluids, and that increases their risk of contracting and spreading bloodborne diseases caused by viruses or bacteria. In this guide to common bloodborne infections from Dr. Najah Doka of ID Care, we answer the question “What are bloodborne diseases?” and explain what you need to know to prevent, diagnose, and treat the most common ones.
The top 3 bloodborne diseases in the United States are:
- human immunodeficiency virus (HIV)
- hepatitis B (HBV)
- hepatitis C (HBC)
These diseases are of special concern to those involved in high-risk sexual behaviors, intravenous drug use, and occupations where workers encounter blood or bodily fluids in the course of their jobs. This can affect workers in healthcare, public safety, funeral or autopsy services, haircutting or cosmetology professions, education, laundry facilities, blood banks, labs, and tattoo parlors.
But other people can contract bloodborne diseases, too, so it’s important for everyone to understand what causes these illnesses and how to avoid becoming infected with them. To stay safe, Dr. Doka advises reading this guide to common bloodborne diseases to know that these conditions:
- are caused by different pathogens whose prevalence varies according to location in the world
- are most likely to affect certain groups based on high-risk lifestyles or occupations, those born to infected mothers, or those immunocompromised
- can be easily diagnosed by a qualified infectious disease doctor
- can be prevented through several proven strategies, such as using condoms during sex, avoiding sharing needles, and wearing personal protective equipment (PPE) in healthcare settings
- can be treated and sometimes cured
- can be deadly if left untreated
What Causes Bloodborne Diseases?
Bloodborne diseases, which affect and can be transmitted through blood or bodily fluids, are caused by bloodborne pathogens. According to Dr. Doka, pathogens are microorganisms that live in blood or other bodily fluids that can cause disease.
In the case of bloodborne diseases, she said, pathogens most commonly fall into one of two categories: viruses or bacteria.
What Are the Most Common Bloodborne Diseases?
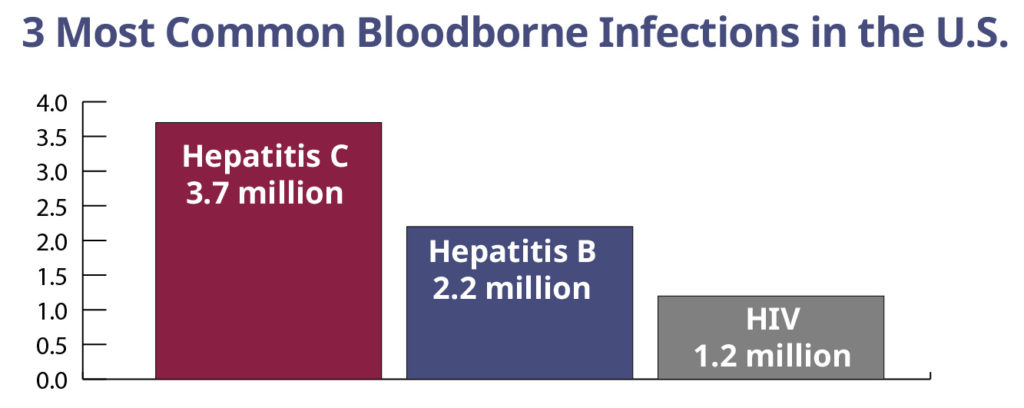
In the U.S., the 3 most common bloodborne pathogens are also the most infectious:
- Hepatitis C (HCV): a virus that causes liver inflammation and affects about 3.7 million Americans, answering the question of which bloodborne pathogen is the most prevalent
- Hepatitis B (HBV): a viral liver infection that affects at least 2.2 million Americans, and is the most contagious bloodborne hepatitis infection
- Human immunodeficiency virus (HIV): a virus that attacks the immune system, can develop into acquired immunodeficiency syndrome (AIDS) if left untreated, and affects at least 1.2 million Americans
“The prevalence of these viruses increases every year and not just because of new infections but because individuals already infected also can develop chronic forms of the disease that must be treated on an ongoing basis,” Dr. Doka said.
Across the world, there are more than 20 pathogens that can live in the blood and cause bloodborne diseases. These include bacterial infections like syphilis and brucellosis, as well as viral hemorrhagic fevers such as Ebola and Lassa fever, which affect multiple organ systems and can cause bleeding. Although many of these are not prevalent in the US, infectious disease doctors like those at ID Care stay current on how to best prevent and treat them so they can advise and care for individuals who travel internationally, especially to high-risk countries.
How Are Bloodborne Diseases Spread?
Individuals commonly contract bloodborne diseases by coming into contact with pathogens in:
- blood
- blood products, such as platelets or fresh frozen plasma (note: this is rare due to screening)
- vaginal secretions
- amniotic fluid
- semen
- pleural fluid from the chest cavity
- joint fluid
- sharing of hypodermic needles
- puncture from needles or sharps in healthcare settings
Although the most prevalent bloodborne diseases are passed through contact with blood or bodily fluids, Dr. Doka also noted that some viruses, bacteria, and parasites that can live in the blood and may be transmitted through bodily fluids, carry a higher risk of transmission through other modes:
- Babesia via tick bite
- MRSA via touching contaminated surfaces/soft tissue wounds
- Zika and malaria via mosquito bite
Who is Most at Risk for Contracting a Bloodborne Disease?
In this guide to common bloodborne diseases, we identify several groups of people who face a higher likelihood of contracting these pathogens than other individuals in the population at large:
- Intravenous drug users, due to the potential sharing of contaminated needles
- Individuals involved in high-risk sexual behaviors, including sex workers or others who have multiple partners
- Babies born to infected mothers, who can contract a bloodborne disease in utero or during birth
- Immunocompromised people, whose immune systems are weakened because they are very young or old, or are taking immunosuppressive medications
- Anyone in contact with an infected person’s bodily fluids through an open wound, cut, or mucous membrane
- Healthcare workers, who may accidentally get stuck with contaminated needles or sharps
How Do You Diagnose Bloodborne Infections?
If the presence of a bloodborne disease is suspected, it’s important that an infectious disease doctor conduct a health evaluation to assess symptoms and carry out required tests. During the appointment, the specialist will:
- Evaluate symptoms. Infection with HIV can bring on persistent fever and flu-like symptoms. Hepatitis B can cause jaundice, nausea, and abdominal pain, while hepatitis C can be elusive, as it is likely to spark mild symptoms or none.
- Conduct blood tests. “This is the definitive way that doctors at ID Care identify bloodborne diseases,” Dr. Doka said. “A blood test can detect the presence of a virus’s DNA or antibodies made by the body in response to infection with any of these illnesses.”
How Do You Prevent Bloodborne Infections?
Dr. Doka and the team of infectious disease doctors at ID Care recommend the following preventative measures to keep the spread of bloodborne infections at bay:
- Avoid recreational intravenous drug use. For those who do engage in this kind of activity, it’s important to never share needles, as that could lead to contact with the blood or body fluids of someone who has a bloodborne disease.
- Engage in safe sexual behaviors. Dr. Doka recommends being monogamous with an uninfected partner or using condoms with partners who may be infected to protect against the spread of HIV, hepatitis B, and hepatitis C — even if these diseases are well controlled.
- Get vaccinated. Of the top 3 bloodborne viruses in the U.S., only one can be prevented through vaccination: hepatitis B. This series of vaccines is available at any stage of life, from newborn through adult.
- Take preventive medications. For those who want to prevent getting HIV or seek protection after possible exposure to the virus, pre- and post-exposure prophylaxis medications are available to protect against development of the disease.
- Take extra precautions during childbirth. When a mother-to-be is infected with a bloodborne pathogen, an infectious disease doctor should continue to treat her, and if it is HIV, in addition to required oral medications, special intravenous medications should be administered during childbirth to help prevent transmission to the baby. “This has greatly increased our success rate when it comes to keeping newborns HIV-free,” Dr. Doka said.
How Can Healthcare Workers Protect Themselves?
Healthcare workers risk contracting bloodborne infections when they handle medical instruments with sharp points or edges or come in contact with the blood or bodily fluids of patients who are infected. That’s why Dr. Doka’s guide to common bloodborne diseases suggests some preventive measures to counter these occupational hazards:
- Provide vaccinations. At many hospitals, workers can offer the preventive vaccine to patients at risk of having or contracting hepatitis B, if these patients have not already received it.
- Suit up. When handling a patient’s bodily secretions, healthcare workers can protect themselves by wearing appropriate PPE, including gloves, gowns, and goggles.
- Get screened. When a healthcare worker accidentally sustains a puncture wound from a contaminated needle or sharp, both the patient and the care practitioner should immediately be screened for hepatitis B, hepatitis C, and HIV to determine their baseline status.
- Seek treatment and follow-up. If a healthcare worker has come in contact with blood or bodily fluids infected with HIV, post-exposure prophylaxis is recommended within 72 hours of exposure. Thereafter, the worker should undergo weekly or biweekly labs to monitor viral status.
What Are the Best Treatment Options for Bloodborne Diseases?
Patients diagnosed with bloodborne pathogens can benefit from seeking the care of infectious disease specialists like Dr. Doka and her colleagues at ID Care, who know how to select the right treatments from a host of options designed to cure these illnesses or keep them in check.
- Treating HIV: For someone who has tested positive for HIV, there are advanced treatment options, so it’s particularly important to consult with an infectious disease doctor. While HIV can’t be cured, it can be treated to the point where the virus is undetectable. “There was a time when we told patients to take 4 tablets 3 times a day, and it was a daunting process,” Dr. Doka said. “Now, we’re down to one easy pill a day. There are several to choose from and they are very tolerable and effective.”
- Treating hepatitis B: During the acute or initial phase of hepatitis B, infectious disease doctors give patients’ immune systems time to eliminate the virus and develop antibodies against it. However, in some patients, the virus converts to the chronic phase, and then the doctors prescribe oral antiviral medications to prevent more aggressive illness that could lead to liver failure.
- Treating hepatitis C: “Over the last couple of years, many new treatment options have emerged, including pills that allow us to cure hepatitis C — something that was unheard of when I was a medical resident,” Dr. Doka said. “This is a great improvement over previous therapies, which were not curative and often included the use of interferon, an injectable drug that did not have the greatest success rate.” To choose the most appropriate treatment, infectious disease doctors conduct tests that determine the disease’s subtype and whether it has progressed enough to cause hardening of the liver.
When caring for patients who have bloodborne diseases, infectious disease doctors also understand the importance of offering a risk assessment designed to detect any simultaneous bloodborne infections, something primary care doctors may not realize is necessary. Dr. Doka noted, “This step is crucial, because these viruses or bloodborne pathogens should not be treated in isolation,” she said. “If someone comes in with hepatitis B, a good infectious disease doctor will also screen them for hepatitis C, HIV, and syphilis, because the coexistence of these viruses can make each of them more aggressive.”
What is ID Care’s Role in Caring for People with Bloodborne Infections?
Due to ID Care’s specialized training as well as experience with the latest developments in the diagnosis and treatment of infectious diseases, these specialists are leaders in the care of patients affected by HIV, hepatitis B, hepatitis C, and other bloodborne diseases. Across ID Care’s 10 New Jersey locations, all 50+ physicians are also well-versed in screening for other simultaneous bloodborne infections, as described in this guide to common bloodborne diseases.
“All of us within the practice are experts in providing preventive hepatitis B vaccines, pre- and post-exposure prophylaxis counseling, and treatment for HIV, hepatitis B, hepatitis C and other bloodborne diseases,” Dr. Doka said. “For those planning travel to different parts of the world, ID Care doctors are also uniquely prepared to provide advice and guidance about the bloodborne pathogens most likely to pose a risk in those regions.”
To schedule an appointment with an ID Care infectious disease expert today, call 908-281-0610908-281-0610 or visit idcare.com.