This article was medically reviewed by Dr. Ira Gurland.
Shingles will affect about a third of all Americans at some point in their lifetime. However, while many people have heard of the disease, fewer know much about it. Because shingles is so common and has the potential to produce painful complications, it’s important for everyone to understand the basics of this viral infection, including its close relationship with chickenpox.
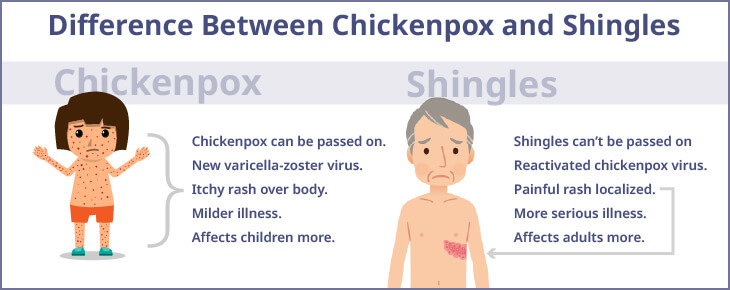
Both diseases have the same origin, but there are important differences. Understanding these distinctions can help avoid confusion:
- Shingles and chickenpox are different infectious diseases, but both are caused by the same virus, called varicella-zoster (VZV).
- Chickenpox symptoms are the body’s first reaction to a varicella-zoster infection, presents as a severe skin rash, is more common in adolescence, and is highly contagious.
- Shingles symptoms are the body’s subsequent reaction(s) to the same varicella-zoster infection that reactivates in the body, often many years later. It is more common in adults and presents as a painful rash as it strikes the nerves. You can’t get shingles from someone who has shingles. However, you get chickenpox from someone who has shingles if you never had the chickenpox vaccine or chickenpox earlier in life.
In this blog, you’ll learn all you need to know about shingles from ID Care infectious disease doctor Ira Gurland, MD, including how to recognize its telltale rash, how vaccination and rash hygiene are essential to prevent transmitting the virus, and how antivirals, pain medications, and topical care can treat an infection if you get one.
What’s the Difference Between Shingles and Chickenpox?
How does the same virus produce two different diseases? Essentially, the body’s immune response changes between the first varicella-zoster infection contracted from another person and the second infection from the dormant virus that remains within your body. The different immune responses lead to different symptoms, contagiousness, and treatment options.
Symptoms of Chickenpox
If you become infected with the varicella-zoster virus, your body will respond first with chickenpox symptoms, usually including headache, fever, sore throat, and a blistering red rash. The rash may cover your entire body and is typically very itchy.
When you recover from chickenpox symptoms within about two weeks, the varicella-zoster virus will remain in your body, lying dormant in a portion of the spinal cord called the dorsal root ganglion. The virus can stay there indefinitely.
Symptoms of Shingles
In some people, the dormant virus reawakens later in life to cause shingles symptoms. Like chickenpox, shingles typically causes headache, fever, and a blistering red rash. However, the shingles blister rash is much smaller and very painful compared to the itchier chickenpox rash.
A shingles rash often looks like a single stripe around the left or right side of the body, but it may also appear elsewhere. “You can get shingles on your face,” said Dr. Gurland, “in your ear canal, on your back, your behind, your leg, your arm — anywhere there’s skin.”
Other common shingles symptoms include:
- Itching, numbness, or tingling before and after the rash appears
- Headache
- Chills
Shingles and Chickenpox Contagiousness Comparison
Chickenpox is very contagious when in close contact with an infected person. Before the FDA approval of the chickenpox vaccine in 1995, it was a very common childhood illness. Since then, chickenpox cases have dropped by more than 99%. However, unvaccinated people who have never been infected can catch chickenpox at any age. Patients are most contagious when blisters are present, and they should isolate during this phase of the disease.
Shingles occurs most commonly in people over 50 years old, but it can strike at any age in unvaccinated people who have already had chickenpox. But you cannot get shingles if you haven’t had chickenpox first. The virus in shingles blisters is not as contagious as in chickenpox blisters, but the varicella-zoster virus (VZV) is still present in the fluid and transmission is possible.
However, you can’t get shingles from someone who has shingles. Direct contact with a person who has shingles can only spread VZV to a person who has never had chickenpox or the chickenpox vaccine. If infected with VZV, they will get chickenpox, not shingles. They can develop shingles later as the virus is now in their body.
“Catching varicella-zoster from a shingles blister is very unusual,” Dr. Gurland noted, “but it’s why I tell all my shingles patients to cover up their rashes. In limited instances, an uncovered rash can become a contagion concern.” It’s also possible to get shingles more than once. According to Dr. Gurland, “it is uncommon, but I’ve seen it happen.” Fortunately, most people who get shingles only get it once.
Diagnosing Shingles Infection
Shingles diagnosis is straightforward: It’s usually identified by a doctor through clinical exam. “Basically,” said Dr. Gurland, “when you examine a shingles patient, you’ll see the characteristic red blistering rash, and most of them will complain of pain near or at the location of the rash.”
In high-risk patients or cases where symptoms are not clear cut, a blood test or blister-fluid test can definitively reveal the presence of the virus.
Can You Have Shingles Without the Rash?
Whether or not shingles can present without a rash is a topic of debate, and for Dr. Gurland, the answer is not simple: “There’s a lot of discussion about this because, without the rash, you’re left with pain at a single nerve root, and other diseases can cause that. But there are people who present with just pain and while you are confident that they have shingles, they just don’t have the typical rash, and they may even respond to some shingles treatments. But it’s a hard diagnosis to make without the rash.” That’s why seeking the care of an infectious disease specialist like those at ID Care is key as experience can play a vital role in the proper diagnosis and treatment of shingles.
What Triggers a Shingles Outbreak and Who Is Most at Risk?
According to Dr. Gurland, “we just don’t know why outbreaks happen — some researchers have linked shingles with periods of excess stress, but most people who get stressed don’t get shingles.”
However, shingles is more common in patients whose immune systems aren’t functioning normally due to cancer, medications, other infections, and other health conditions. “While you don’t need an immune deficiency to get shingles,” said Dr. Gurland, “a significant minority of patients who have it also have a suppressed immune system.” The risk also increases with age (50+), although Dr. Gurland has seen very young patients develop the disease as it doesn’t discriminate.
Why is Shingles Painful?
After first causing chickenpox, the varicella-zoster virus lies dormant in the dorsal root ganglion, which is also the pain center of the spinal cord. It’s where your sensory nerves meet up before heading to the brain. So, every portion of your body has a corresponding portion of the spinal cord that controls its pain. An area of skin whose sensory nerves form a single nerve root is called a dermatome.
According to Dr. Gurland, “when that nerve root gets irritated by the shingles virus, it sends pain signals to the brain that make the corresponding dermatome or skin region hurt. This is called neuropathic pain, and it’s notoriously harder to treat than more common types of pain like a toothache.”
Shingles pain tends to be worst on the more sensitive portions of the body. The face can be particularly painful, as a single nerve root there concentrates the sensitivity. A rash on the back or belly would be less painful because the nerve endings there are more diffuse, but it would still be unpleasant at best.
Typically, shingles is most painful within 4-5 days of the onset of symptoms and the blistering rash and then it can begin to dissipate as the blisters scab over, which can take 7-10 days (and longer to clear). But for some patients, significant pain can last much longer – weeks, months, and rarely it can lead to lifelong pain. The entire course of shingles usually takes from 3-5 weeks to recover and the rash to totally clear, but this can differ by person.
What Are the Complications of Shingles?
The main shingles complication of concern is ongoing postherpetic neuralgia (PHN), which is long-duration pain related to shingles. Because the shingles virus lives in the sensory portion of the spinal cord, when it persists in an active state, the resulting long-term pain can be debilitating and lead to downstream effects such as anxiety, depression, insomnia, and weight loss.
“Shingles pain, or PHN, typically doesn’t respond well to over-the-counter treatments like Tylenol or Advil,” said Dr. Gurland, “and prescribed pain medications are not much better. That’s what everybody fears most about shingles.”
In rare cases, shingles can affect unexpected parts of the body, including the eye, where it is called herpes zoster ophthalmicus (HZO). It can result in visual impairment issues, chronic pain, and related conditions and is cause for immediate medical intervention.
Can Shingles Be Prevented?
Shingles cannot be cured, but it can be prevented and treated. The best preventative measure for shingles is to get vaccinated. The vaccine is called Shingrix, and it has proven effective at blocking shingles and even more effective at reducing the severe pain associated with it.
When it comes to who should get the shingles vaccine, Dr. Gurland recommends it for everyone over age 50. It is delivered in 2 doses, with 2 to 5 months between the first and second injections, which are no more painful than typical flu shots. After the first shot, people tend to experience very few side effects. After the second shot, you might have a fever or feel achy for a day or 2.
“We want to make shingles a very rare disease,” said Dr. Gurland, “and right now it isn’t. We can fix that by vaccinating people, so my top 3 things to remember about shingles are to get vaccinated, get vaccinated, and get vaccinated.”
It’s uncommon, but some vaccinated people have gone on to get shingles. However, the vaccine still helps alleviate the severe postherpetic neuralgia pain that people find most worrisome. According to Dr. Gurland, “while the vaccine prevents shingles to a significant degree, you really want to be vaccinated to avoid the postherpetic neuralgia.”
Other measures that can help prevent varicella-zoster infection include basic infection control practices such as avoiding contact with anyone known to be infected with chickenpox or shingles and washing your hands often.
If you do experience a shingles outbreak, you can help prevent spreading varicella-zoster virus to others at risk by:
- Covering the rash
- Not touching or scratching the rash
- Washing your hands often
You should also avoid contact with immune-compromised people until the rash crusts and blisters are no longer apparent. These include premature and low birth weight newborns, unvaccinated pregnant women who’ve never had chickenpox, and people affected by chemotherapy, organ transplant, or HIV.
Can You Go to Work with Shingles?
If the rash can be covered with a bandage or clothing and there’s not too much pain, most people can continue to work during a shingles outbreak. If the rash is on your face, however, it’s probably best to stay home until it resolves.
Dr. Gurland advises that “while you can generally go to work if your rash can be covered, those who work in hospitals, nursing homes, and other care facilities should check their employee health policies about when to return to work to avoid potentially exposing immune-suppressed patients in their care.”
Shingles Infection Treatment
The major drugs used to treat shingles are prescription antiviral medications that interrupt the virus’ ability to multiply in the body. These medications include Acyclovir, Famciclovir, and Valacyclovir and they all use a similar mechanism of action to interfere with viral replication. It’s important to seek treatment soon after the onset of shingles symptoms, as the medications work best if given within the first three days of onset of symptoms.
In addition to antiviral drug treatment, shingles symptoms can be mitigated by:
- Keeping the rash loosely covered with a non-adhesive sterile bandage
- Cooling the area with ice packs, wet cloths, or cooling baths
- Wearing loose-fitting, natural fiber clothes to prevent painful skin irritation
Although treatment will send shingles back into remission in the spinal cord from which it emerged, the virus will remain there with the potential to come back and cause the disease again — although that is uncommon.
What is ID Care’s Experience Caring for Shingles Patients?
“There are over 50 physicians at ID Care across 10 New Jersey locations, and our team keeps growing,” said Dr. Gurland, “including advanced care providers with broad experience treating patients with shingles, and who understand exactly how the disease progresses, how to fight it, and how to keep it from coming back.”
When Should You See an ID Care Doctor for Shingles?
“If you think you might have shingles, if you’re concerned about pain associated with shingles, or if you’re unhappy with your current shingles treatment plan, you should see a specialist at ID Care,” Dr. Gurland said. If you can get to a doctor within 72 hours of the onset of symptoms, you’ll have the best chance for a good result.
At ID Care, your health is our priority. To schedule an appointment to get your shingles vaccine or to consult with an infectious disease doctor today, call 908-281-0610 or visit https://idcare.com.