This article was medically reviewed by Dr. Najah Doka.
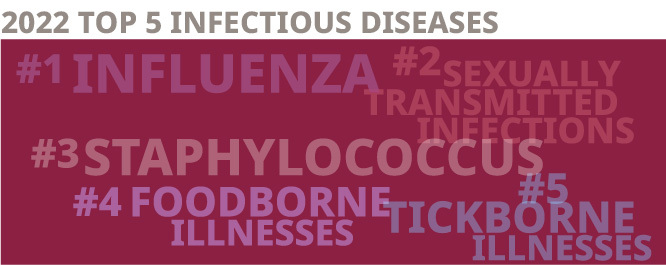
While the global COVID-19 pandemic is foremost in everyone’s mind, it’s easy to forget about the other infectious diseases that can threaten good health — but they have not gone away. In fact, some are on the rise. As the new year begins, it’s a good time to review the top 5 infectious disease concerns to watch out for in 2022. ID Care infectious disease specialist Dr. Najah Doka explains how to avoid, diagnose, and treat the most common current non-COVID infections, including:
- Influenza (Flu),
- Sexually Transmitted Infections (STIs, STDs, VD)
- Staphylococcus (Staph)
- Foodborne Illnesses
- Tickborne Illnesses
Understanding these diseases and taking effective steps to prevent their transmission can give you the best chance for a healthy 2022.
What is an Infectious Disease?
The past two years have been filled with concerns about the infectious disease we know as COVID-19, including the most contagious variant so far, Omicron; but other infectious diseases remain active as well.
According to Dr. Doka, “an infectious disease is a communicable illness caused by pathogenic microorganisms including bacteria, viruses, parasites, and fungi. It becomes a public-health concern when the transmission rate is high enough that it expands from a personal or family health issue and becomes a community-wide threat.”
#1 Influenza / Flu
Commonly known as the flu, influenza is a virus typically spread through respiratory droplets exhaled by people carrying the infection. These are the most common seasonal flu viruses we’re likely to face:
- Influenza A virus (IAV) can spread from animals to humans and is the most common form we encounter. It is also the variant responsible for influenza pandemics.
- Influenza B virus (IAB) produces symptoms much like type A, but can only pass among humans, not other animals. It can cause seasonal outbreaks during “flu season” from September to April but remains a threat at any time of year.
- Influenza C virus (IAC) is the mildest form, producing the least severe disease.
Because flu shares some symptoms with other respiratory infections, Dr. Doka recommends a medical examination for anyone with signs of flu. “An infectious disease doctor would be the best choice,” she said, “to get an accurate flu diagnosis and a flu treatment specifically designed for it.”
In addition to evaluating your symptoms, a doctor may administer a rapid antigen test, which involves taking a swab sample from the back of the nose or throat.
Flu symptoms usually include some combination of the following:
- Fever
- Cough
- Sore throat
- Runny nose
- Body aches
- Headache
- Chills
- Fatigue
While more severe cases may require medication, flu treatment for patients with milder cases usually involves isolation at home to prevent spread, rest, and over-the-counter remedies to relieve flu symptoms.
Patients are most likely to transmit the disease to others during the first 3 to 4 days of flu symptoms, but Dr. Doka warns “you can still be contagious as much as 7 or 8 days later.”
Certain high-risk groups are particularly susceptible to catching influenza and suffering the most severe symptoms, including death. These include older people, pregnant women, and people with compromised immune systems regardless of cause.
Flu prevention entails the general infection control measures of washing hands, social distancing and avoiding close contact with people known to have the disease, but according to Dr. Doka, “the most effective way to prevent influenza is through vaccination, so be sure to get your seasonal flu vaccine.”
#2 Sexually Transmitted Infection / STI, STD, VD
Sexually transmitted infections (STIs), also known as sexually transmitted diseases (STDs) or venereal disease (VD), have been on the rise recently, and should be a concern for all sexually active people.
They are typically spread by genital area skin-to-skin contact, or by contact with bodily fluids such as semen and vaginal secretions. Sexually transmitted disease symptoms and infection may be prevented by abstaining from sex, using condoms, or ensuring that all sexual partners involved are medically tested and proven to be infection-free prior to sex. STIs come in many forms, but the most common ones in the United States are:
- Chlamydia
- Syphilis
- Hepatitis B
- Gonorrhea
- Human Papillomavirus (HPV)
- Genital Herpes
- HIV/AIDS
Chlamydia
Currently, chlamydia is the most common bacterial STI moving through our communities. While it can infect people of any age, it is most often diagnosed in people between 20 and 25 years old.
According to Dr. Doka, chlamydia can present with symptoms including “discharge, pain, and a burning sensation upon urination, but generally not lesions or other indications on the skin. In some cases, patients have no symptoms at all, and this raises the transmission risk to their partners.” People in the most jeopardy of catching chlamydia include those with a new partner and those with multiple partners.
The disease does more damage the longer one has it, whether symptoms are noticeable or not. “For example,” warns Dr. Doka, “if untreated, women with chlamydia can develop pelvic inflammatory disease, or PID. It can cause reproductive problems and lead to complications with pregnancy.”
Fortunately, chlamydia is easy to diagnose and treat. Those who have symptoms or suspect an exposure should see an infectious disease doctor, who will evaluate the patient’s history and conduct a physical exam and lab test. “Don’t delay seeing the doctor, because early diagnosis and quick treatment produce the best outcomes,” Dr. Doka advises, adding, “treatment is usually with antibiotic pills with no need for hospitalization, and patients recover quickly.”
Syphilis
Syphilis is less prevalent than chlamydia now, but it can have very serious long-term effects. Patients are diagnosed with one of the four progressive stages of the disease, and if left untreated, it can cause brain damage and terrible problems with the eyes, heart, nerves, brain, liver, bones, and joints. Women with long-term syphilis can give birth to stillborn or developmentally delayed babies.
Who Should You See for an STI?
If you suspect any STI, Dr. Doka recommends seeing an infectious disease specialist. A family doctor may be able to help with a particular STI, but an infectious disease doctor will broadly analyze a patient’s risk factors and lifestyle as well as conduct tests to see if other likely infections are present.
“If someone comes to me with chlamydia, I don’t just treat the chlamydia,” she said, “I also screen them for syphilis, HIV, hepatitis, and herpes, because these infections all bear the same risk factors. If we find them, we treat them, and if not, we rule them out.”
Additional information on STDs can be found here from ID Care specialists who care for patients with these conditions.
#3 Staphylococcus Infection / Staph
Staph infections remain a concern in 2022, because the bacterium never went away, it’s just been overshadowed by COVID-19. In Dr. Doka’s view, “Staph is still a big problem.”
The infection produces a range of symptoms with different levels of severity:
- Superficial skin infections with cellulitis (redness, swelling, and pain)
- Boils and furuncles (infected hair follicles) at deeper levels
- Bloodstream infections that can damage heart valves
According to Dr. Doka, “Staph diagnosis involves a physical examination and a bacterial culture to confirm the type, and the most common are skin and soft tissue infections.”
In the worst-case scenario, patients can contract MRSA (Methicillin-resistant Staphylococcus aureus), which is resistant to certain antibiotics. This makes Staph treatment more difficult, and transmission easier. MRSA targets people living or working in close quarters, such as homeless shelters, sports team locker rooms, daycare centers, and family dwellings.
When Staph is in a household, family members should stop sharing towels, sheets, and blankets, and avoid physical contact with infected people. When multiple family members are infected, Dr. Doka prefers to treat them together, which includes active infection treatment followed by a decolonization protocol to minimize recurrence.
Early Staph diagnosis improves treatment outcomes, so Dr. Doka advises people with symptoms to “get evaluated as soon as possible, because starting Staph treatment quickly will make a big difference.”
Treatment usually involves oral or intravenous antibiotics. However, not every physician is skilled in choosing the right antibiotic for these infections, so Dr. Doka recommends seeing an infectious disease specialist for the best care.
#4 Foodborne Illnesses
Number 4 of the top 5 infectious disease concerns to watch out for in 2022 is a familiar one, foodborne illnesses. Many pathogens can cause it, but diagnosis of various foodborne illnesses has revealed viruses and bacteria as the main culprits. They can contaminate food at any point in the long journey that leads to your mouth: from the agricultural areas where food is grown, from the workers who process and transport it, from the cooks who prepare it, and from the wait staff or family members who brings it to your table. Even the person who eats the foods may contaminate it if proper care is not taken.
Foodborne illness symptoms are often similar, consisting of diarrhea (sometimes bloody), vomiting, stomach cramps, and fever. In the US, the most common foodborne pathogens are:
- E. coli comes from the intestinal tract and can enter the food stream due to cross contamination during the butchering of livestock. Severe E. coli can cause renal failure.
- Salmonella is less common, but on the rise. Humans become infected through contaminated food or water.
- Norovirus is the most easily transmissible foodborne illness and has caused many recent outbreaks on cruise ship.
- Hepatitis A is commonly passed as a foodborne illness, however, there is a vaccine available to prevent its spread.
- Campylobacter can be a local contaminate but is more often seen in foods imported from regions with substandard anti-contamination protocols.
For the individual food consumer, the best prevention for a foodborne illness is proper hand and food hygiene: wash hands, utensils, fruits, and vegetables before eating, and be sure to cook animal products such as meat to the right temperature. Also, refrigerate leftovers within two hours to prevent recontamination.
If you experience foodborne illness symptoms beyond a day, seek medical attention from an infectious disease doctor. In severe cases, go to the emergency room for foodborne illness treatment and intravenous rehydration.
#5 Tickborne Illnesses
The last of the top 5 infectious concerns to watch out for in 2022 is tickborne illnesses. Ticks infected with viral and bacterial pathogens are an ongoing challenge for infectious disease doctors in New Jersey and anywhere in the northeastern United States, particularly because tickborne illness symptoms tend to overlap. Peak times for tick activity are the warmer months of spring, summer, and fall, but you may encounter a live infected tick at any time of year.
Lyme Disease
The most common tick-borne illness across the region is Lyme disease. It is transmitted primarily by the deer tick, after biting into skin and remaining attached for at least 48 hours. Dr. Doka reports that “the recipe for prevention is straightforward: don’t let a tick bite you, and if it does, remove it as quickly as possible.”
You can best accomplish this by avoiding the natural areas that ticks prefer: woods, fields, and patches of overgrown brush or grass. This can include a typical suburban lawn or garden. If you intend to enter these areas, dress in long sleeves, socks, and pants, covering as much exposed skin as possible. “This can be difficult when it’s very hot,” said Dr. Doka, “but it’s worth the effort.”
Remember to visually inspect your clothing and remove any ticks you find. Wearing light-toned clothing can help you better see these small dark brown or black insects.
As soon as you return home, conduct a full naked-body tick check. A very close relative or friend can help inspect hard-to-see parts. If you’re alone, a mirror can be a big aid. Pay close attention to crevices, folds and areas covered with hair, especially around your midsection, genital area, and armpits where ticks like to feed.
Dr. Doka noted, “If an infected tick is attached for fewer than 24 hours, the chance of Lyme transmission is very low. Beyond that, the risk increases.” If you find an attached tick, remove it with tweezers by firmly grasping its head and slowly pulling it out. If it comes apart, remove all the parts. If you have trouble, a medical professional can help.
A common Lyme symptom is a bulls-eye rash at the point of infection, but many patients may miss it. After that, you may have flu-like symptoms in the short-term, but long-term Lyme can cause serious, debilitating health consequences including arthritis and carditis (heart inflammation). Fortunately, quick treatment with the right antibiotic can eliminate the disease. “Take it seriously,” warns Dr. Doka, “Lyme disease is no joke.”
Babesia & Others
A lesser known but serious tickborne pathogen is Babesia, which can cause anemia and serious problems for immunocompromised people. It’s important to consider because the tickborne illness treatments for Babesia and Lyme are very different, even though they share many symptoms. This is where screening by an infectious disease doctor is particularly valuable. They can distinguish among the common infections and atypical ones like Anaplasma, Ehrlichia, and Rocky Mountain Spotted Fever to make a proper tickborne illness diagnosis and proper tickborne illness treatment plan.
ID Care’s Role in Addressing the Top 5 Infectious Diseases in 2022
ID CARE is an invaluable resource for the management of these top 5 infectious disease concerns to watch out for in 2022. With more than 50 infectious disease doctors with locations throughout New Jersey, ID CARE can see many patients at one time and has the skills to treat them all. “The practice also works to educate the communities it serves. We see patients in our offices, in hospitals, and in nursing facilities,” said Dr. Doka, “to prevent, diagnose, and successfully treat these infectious diseases for the best possible outcomes.” To schedule an appointment with an ID Care infectious disease expert today, call 908-281-0610 or visit idcare.com.