Tips for managing pertussis in babies & elderly adults including recognizing whooping cough symptoms
The “sandwich generation” – people caring simultaneously for both children and elderly relatives such as aging parents – face every-day challenges, strain and fatigue from juggling family members’ needs, along with financial pressure.
Whooping cough can intensify those challenges and presents a double concern for sandwich generation caregivers: It’s a dangerous infectious disease for children – especially infants – and the elderly, even if seniors are not living with you. Understanding whooping cough symptoms helps caregivers determine when to seek treatment to prevent serious illness.
This blog covers the top six things sandwich generation caregivers need to know about whooping cough (pertussis):
- What whooping cough is.
- How long pertussis lasts, including when someone is contagious.
- What symptoms to look for in each generation.
- When to seek medical help for whooping cough in babies and elderly.
- Prevention begins with the whooping cough vaccine.
- How to provide effective pertussis treatment at home.
ID Care has more than 50 highly skilled infectious disease physicians, a broad medical support staff of nurse practitioners and physician assistants, and a commitment to patient-centric empathetic care. Our mission is to lead in the prevention, diagnosis and treatment of infectious diseases. Make us your source for excellent infectious disease care:
1. What is pertussis, also known as whooping cough?
Pertussis, more commonly known as whooping cough because of its sound, is a very contagious infection that affects the respiratory system. It’s caused by the bacteria Bordetella pertussis that settles in the mouth, nose and throat of someone who is infected.
People of any age can come down with pertussis, but the illness is especially dangerous for older adults and babies under 1 year old. About a third of infants younger than 1 year old who develop the disease require hospital care, according to the Centers for Disease Control and Prevention (CDC).
Whooping cough is mostly spread by droplets expelled during coughing and sneezing. This puts families spending time together and sharing breathing space at increased risk.
Treating the cough early with antibiotics can make the disease less serious. This is why knowing the symptoms is important, so you can get professional care.
Related Listening From U.S. Food & Drug Administration: What whooping cough sounds like
2. How long does whooping cough last? And when is someone contagious?
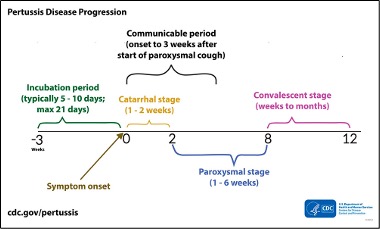
The 4 stages of whooping cough: incubation, catarrhal, paroxysmal and convalescent
The disease progresses in four stages (see diagram below).
8–12 weeks: Decreased coughing with flare ups; convalescent stage.
5-10 days before whooping cough symptoms: Incubation period.
After symptoms begin:
- 8–12 weeks: Decreased coughing with flare ups; convalescent stage.
Whooping cough symptoms in each phase
During the incubation period, there are no symptoms.
In the catarrhal stage, symptoms are mild and similar to a common cold. This stage lasts 1–2 weeks and is when the disease is most contagious. Often people don’t know they have whooping cough and unknowingly spread it to others.
The paroxysmal stage involves violent coughing that can’t be controlled (paroxysms). This stage can last for weeks and is when the distinctive “whoop” is present, which is caused by inhalation after the cough.
In the convalescent stage, which can last weeks or months, the coughing decreases. It can also flare back up over the course of convalescence.
3. What are whooping cough symptoms in younger and older generations?
Whooping cough symptoms in babies and children
In babies and children, pertussis typically begins 5-21 days after exposure with mild cold‑like symptoms. The New Jersey Health Department reports that 4 out of 5 infants catch the disease from someone at home.
Many babies don’t cough at all. Their telling whooping cough symptom is apnea or a general struggle to breathe. Infants are most at risk from whooping cough and need professional care as soon as possible. About a third to a half of infants with pertussis are hospitalized, most often those younger than 6 months. Earlier treatment can prevent that.
Unvaccinated infants and those whose mother didn’t receive the Tdap vaccine during pregnancy are at greater risk of severe complications and death. Complications from pertussis include the following:
- Apnea (a life-threatening breathing pause), which is the most common complication in infants, affecting 68% of babies with the infection.
- Pneumonia, developing in about 22% of infants with pertussis.
- Convulsions, which affect approximately 2% of infected infants.
The CDC says 1% of infants die from complications described above.
Pertussis symptoms in the elderly
In older adults pertussis may present as a persistent cough lasting weeks. They often don’t experience the “whoop” cough, making it easy to miss. Symptoms can include prolonged coughing fits, post‑fit vomiting, fatigue, sleep disturbance and weight loss.
Elderly adults with chronic conditions (especially respiratory and cardiac issues), weakened immune systems, and lifestyle factors such as smoking and obesity are at greater risk of complications. Pneumonia is a serious complication in adults 50 and older with pertussis. Other complications include rib fractures from coughing, passing out, urinary incontinence, eye and brain bleeding, and stroke or encephalitis (inflammation of the brain) in rare cases.
Hospitalization rates increase with age. As many as 14% of those with whooping cough older than 75 are hospitalized. A study in Infectious Diseases and Therapy shows that adults over 50 with pertussis experience high rates of medical care and costs.
Later stage whooping cough symptoms for children and adults
- Uncontrollable, rapid, violent coughing fits (paroxysms), lasting 1-10 weeks with increasing intensity.
- The high-pitched whoop sound when inhaling after a coughing fit.
- Being very tired after fits but feeling better in between them.
- Vomiting during or after fits.
- Struggling to breathe.
- Trouble sleeping.
4. When to seek medical care for pertussis
Get emergency help immediately for anyone having difficulty breathing!
If you suspect whooping cough, which may be the case when cold symptoms last for a week or two, seeing a doctor can result in a definitive diagnosis and the start of antibiotics.
Be sure to see an ID Care specialist:
- If violent coughing begins.
- For infants under 12 months with confirmed or suspected pertussis. This is due to the high rates of hospitalization and complications in infants.
- For elderly adults with whooping cough who have pneumonia or underlying conditions such as heart, lung, immune or neurologic problems. Also seek care if their condition deteriorates quickly.
5. How to prevent whooping cough: Get the whooping cough vaccine
Without doubt, the whooping cough vaccine is the most important step in prevention. Two combination vaccines protect against the disease, DTaP (diphtheria, tetanus and pertussis) and Tdap (this has lower doses of diphtheria and pertussis antigens than DTaP). DTap is for children under 7; Tdap is for older children and adults.
CDC and ID Care recommend these guidelines for vaccination
- Infants and children under 7 receive one dose at five intervals from 2 months old through 6 years old.
- Adolescents should get one dose of Tdap at 11 to 12 years of age.
- At each pregnancy, the mother should get one dose of Tdap during 27 to 36 weeks of gestation.
- Adults who have never been vaccinated can receive a dose of Tdap at any time. Vaccination is particularly important for adults with comorbidities, such as diabetes, chronic respiratory disease, immunodeficiency and obesity.
Other prevention tips
These are particularly important for households with infants and elderly adults.
- Consider wearing a mask in crowded places.
- Avoid sharing space with anyone who has whooping cough.
- If you have symptoms, stay away from high-risk individuals such as the elderly and babies.
- Wash your hands frequently with soap and warm water.
- Stay home until 3 weeks after coughing begins or until 5 days after taking antibiotics.
- Cover you sneezes and coughs and dispose of tissues immediately.
- Consider wearing a mask in crowded places.
6. Pertussis treatment at home
It’s important to treat whooping cough early – if possible before the coughing fits begin. Primary treatment is with antibiotics. This kills the bacteria and can make the illness less serious, last a shorter time and aids in preventing its spread to others.
Antibiotics are not effective after 3 weeks of illness, even if the person still has symptoms. At this point, the bacterial infection has already left the body; the person continues experiencing symptoms due to airways damaged by the disease.
Some people should take preventive antibiotics if they are around others with pertussis. Caregivers should consult their medical provider about preventive antibiotics.
Home remedies for whooping cough
Don’t use cough medicines unless your doctor recommends it. While this seems like a natural home treatment, it is not effective and generally isn’t appropriate for young children. Follow these steps for home care.
- Take antibiotics as your doctor prescribes.
- Get plenty of rest: a quiet, darkened bedroom can help.
- Drink plenty of fluids like water and juice.
- Eat small, more frequent meals to prevent vomiting after coughing fits.
- Try to eliminate irritants in your home that can trigger coughing, such as tobacco smoke, chemical fumes and dust.
