This article was medically reviewed by Dr. Andrew Lee.
If you get COVID-19 and your immediate concerns are about missing work or an important social event, your perspective may be a bit shortsighted. A more troubling issue is the potential longer-term cardiovascular effects of the virus. It has been shown that even a year after having the COVID infection, your risk of having heart problems remains heightened — even if you were previously healthy and never hospitalized for COVID-19 treatment.
With nearly 60% of Americans having had the coronavirus and the vast majority expected to get it, the risk of cardiac issues after contracting this infectious disease is something everyone needs to understand. In this Guide to COVID-19 and Cardiac Issues, ID Care’s Dr. Andrew Lee explains what you need to know to recognize potential heart problems that COVID can cause and to receive the appropriate diagnosis and treatment.
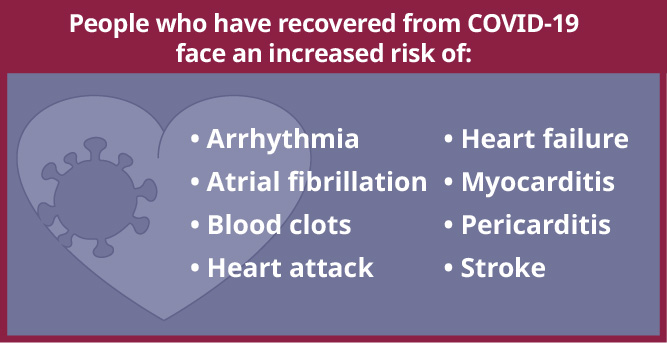
Researchers believe that between 4% and 7% of people who’ve had COVID-19 will develop “long COVID,” meaning that, three months or more after becoming ill, they will experience continuing or new virus-generated symptoms that may include cardiovascular problems. A large 2022 study on the long-term cardiovascular outcomes of COVID-19 published in Nature Medicine shows that, one year after getting sick, people who have recovered from COVID-19 face an increased risk of:
- Arrhythmia, or changes to the heartbeat’s rhythm.
- Atrial fibrillation, a speeding up of the heartbeat in a specific pattern.
- Blood clots in the lungs or legs.
- Heart attack, also known as myocardial infarction, caused by a lack of blood flow to the heart.
- Heart failure, or the inability of the heart to adequately pump blood.
- Myocarditis, characterized by inflammation of, or damage to, heart muscle.
- Pericarditis, chest pain due to inflammation of the sac surrounding the heart.
- Stroke, a reduction or blockage of blood to the brain.
But how does COVID-19, a respiratory virus, damage the heart? Infectious disease doctors like those at ID Care understand that the virus can enter heart cells, where it causes inflammation. Over time, that inflammation can affect the inner surfaces of veins and arteries and damage blood vessels, potentially creating clots that compromise blood flow.
“Heart complications can affect anyone who has had COVID-19, even those who were asymptomatic. However, this most often occurs when people are admitted to the hospital hypoxic — with low blood oxygen that can cause shortness of breath — because then the heart must work harder to pump blood,” Dr. Lee said. “Stress cardiomyopathy brought on by inflammation can stun the heart, reducing its function in the moment or down the line. Alternatively, COVID-19 can spark a cytokine storm, an aggressive immune system response that is meant to kill the virus but can also severely damage healthy heart tissue.”
Fortunately, most COVID-19 cardiac complications are treatable, and some are reversible, particularly myocarditis and stress cardiomyopathy.
COVID-Related Heart Problems: Risk and Prevention
According to the findings of the Nature Medicine study, no subgroup of the population is immune from an increased risk of heart complications following COVID-19. Even athletes and non-smokers with normal BMIs who were free of chronic illnesses such as kidney disease or diabetes were found to have a higher likelihood of heart problems after having COVID-19 compared with people who had similar characteristics but had never contracted the virus.
Importantly, the study did not determine whether being fully vaccinated against COVID-19 makes a significant difference in protecting against these complications. But infectious disease experts widely believe that full vaccination against COVID-19, along with masking and social distancing, are the best ways to avoid contracting or becoming severely sick from the virus.
In fact, since vaccines against COVID-19 were introduced, the infectious disease doctors at ID Care have observed that their unvaccinated patients — along with older individuals who had pre-existing cardiac problems or struggled through severe COVID-19 — are the most likely to become coronavirus “long haulers” with ongoing heart complications.
“Something that appears to meaningfully increase risk is a patient’s hospitalization for a long time with COVID-related hypoxia, because being on a ventilator takes a toll on the heart,” Dr. Lee said. “The heart is working under enormous stress while other muscles weaken from lack of use, so the body can’t provide sufficient energy to support cardiac function. As a result, patients hospitalized for COVID-19, whether they’re vaccinated or not, are often given preventive treatment with high-dose blood thinners.”
Preventing Long COVID with Paxlovid
Are there other ways to help prevent COVID’s most severe long-term symptoms? For some people in the early stages of the virus, a new medication can help. Paxlovid is a prescription oral antiviral drug that reduces the risk of hospitalization and death for patients with mild to moderate COVID-19 who are at risk of disease progression and severe illness. While Paxlovid does not prevent heart disease, its use may result in fewer patients experiencing hypoxia, ventilation, and the heart problems that can follow.
“Paxlovid is not for everybody, because it can cause interactions with some drugs and can generate side effects such as a metallic taste in the mouth,” Dr. Lee said, “but if you’re older and have heart disease or other medical problems such as COPD or atrial fibrillation, you should consider it. If you meet the criteria for Paxlovid but are told not to take it because of anticipated drug interactions, we will often recommend that you go to the emergency room for treatment with a monoclonal antibody.”
Does the COVID-19 Vaccine Cause Heart Problems?
MRNA vaccines against COVID-19, such as those made by Pfizer and Moderna, are widely recommended as a way to prevent severe complications of the virus. However, there is evidence that these inoculations can, in extremely unusual cases, cause myocarditis or pericarditis, particularly in young adults. So, is it wise for this population to get the COVID-19 vaccine?
“Myocarditis related to the vaccine in this population is still extremely rare, so we do recommend the vaccine for young adults,” Dr. Lee said. “A recent study noted that the risk of myocarditis and pericarditis is still much lower for young people vaccinated against COVID-19 compared with those who get the virus itself.”
Is it COVID or is it a Heart Attack?
Because of their increased risk of heart problems, people who have contracted COVID-19 may assume they’re in the grips of a heart attack if they experience chest pain and shortness of breath. But as you will learn in this Guide to COVID-19 and Cardiac Issues, that is usually not the case.
Since the beginning of the pandemic, infectious disease doctors like those at ID Care have learned to look at chest pain and shortness of breath in the context of other symptoms to help determine who is truly experiencing a heart complication. They have found that, in COVID long haulers, chest pain and breathlessness are often part of a constellation of symptoms that can include chronic fatigue, headaches, heart palpitations, and cognition problems. On the other hand, those having heart attacks are likely to have pain that radiates down the arm, back or neck, along with excessive sweating, nausea and/or dizziness.
“Diagnosing these patients can be tricky for doctors who are not experts in this area, because some of the symptoms of long COVID can mimic a heart attack,” Dr. Lee said. “Fortunately, a small 2021 study of patients hospitalized with severe COVID-19 helped us distinguish between people who do and do not have heart complications. Although EKGs in some viral cases suggested heart attacks, angiograms showed that these patients did not have blocked arteries. In addition, it’s important for doctors to check levels of the cardiac enzyme troponin which rises in heart attack patients while the hormone BNP usually rises in heart failure patients.”
How are Cardiac and Other Long COVID Symptoms Treated?
Patients who have even minor post-COVID symptoms that might signal heart irregularities should immediately set up an appointment with a cardiologist. These specialists can not only confirm that symptoms are heart-related but can offer appropriate treatments across a broad variety of options, including medications; surgical, catheter, or stent procedures; and electrical cardioversion, which uses an electrical current to reset the heart’s rhythm.
If cardiac issues are ruled out, patients can seek other treatments for their long-term COVID-19 symptoms, turning to infectious disease doctors like those at ID Care, or to primary care providers or clinics created specifically for COVID long haulers. Treatments may involve breathing exercises; physical, nutritional, or mental therapy; or medications such as steroids or targeted drugs that aim to ease inflammation, with doctors collaborating as necessary with pulmonologists, neurologists, ENT (ear, nose, throat) specialists, or others.
Since the phenomenon of long COVID is so new, researchers are still looking for answers about how to best resolve symptoms. As a result, many therapies are experimental and only available through clinical trials. Interested patients can look online for opportunities or ask their infectious disease doctors for guidance about how to find and enroll in trials of treatments such as antiviral therapies, immunosuppressive drugs, or convalescent plasma harvested from patients who have recovered from COVID-19.
How Does ID Care Help People with Post-COVID Cardiac Issues?
When patients develop cardiac symptoms or potential long-term heart disturbances due to COVID-19, the infectious disease doctors at ID Care are prepared to help them by:
- Connecting them with a cardiologist who can diagnose, treat, and monitor cardiac illnesses.
- Suggesting lifestyle changes for at-risk patients, such as smoking cessation and a diet low in salt and cholesterol to help prevent heart problems or keep them in check.
- Encouraging compliance with basic health measures, from keeping doctors’ appointments and adhering to medications to sticking with lifestyle changes long-term.
There is no test that identifies long COVID, so if symptoms exist without the presence of heart complications, the infectious disease doctors at ID Care rely on a patient’s health history and a clinical exam to connect the dots. The practice includes more than 50 doctors, all of them well-versed in identifying long COVID, whether in their 10 offices or in the many hospitals across New Jersey. In addition to being expert diagnosticians, ID Care doctors have a breadth of experience in treating patients with COVID and knowing who to refer them to if advice from another specialist is needed.
Beyond working with patients who are living with the long-term effects of COVID-19, doctors at ID Care offer 24/7 expertise in preventing, diagnosing, and treating people with all kinds of infectious diseases, including those contracted during international travel and those that can benefit from treatment with outpatient infusion therapy. To schedule an appointment with an ID Care infectious disease doctor today, call 908-281-0610 or visit idcare.com.