This article was medically reviewed by Marsha Kallich, MD (retired December 2023).
Lyme disease is important because it’s a widespread, easily acquired tickborne infection that can have long-term health effects. The CDC reports that nearly half a million Americans are treated for Lyme every year. The spring and summer months coincide with “tick season,” when the lure of outdoor fun with lots of exposed skin can pose an increased risk for Lyme transmission.
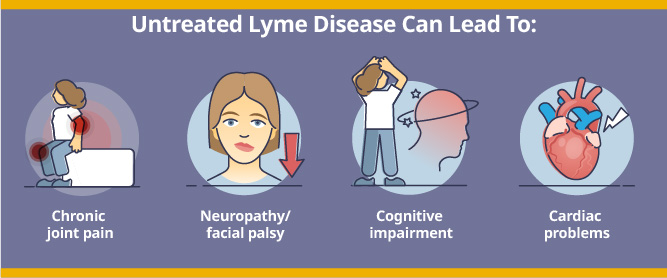
Spread through the bite of infected deer ticks, some infections start with flu-like symptoms, but not all have that as the initial clue. The telltale bull’s eye rash may occur in 70 to 80% of infected people. It can move into joints and organs, leading to a variety of problems, including:
- Neurological symptoms like neuropathy and facial palsy
- Heart block of the electrical system and other cardiac problems
Named for the town of Lyme, Connecticut where it was first described in 1975, Lyme disease has since spread outward and is now a nationwide concern. It is endemic across the northeastern United States.
New Jersey is in the heart of the hot zone, and Lyme can be a dangerous tickborne threat in our region. People have wondered – is Lyme disease fatal? In very rare cases, it can be, but that question has been a source of controversy. Depending on which group is scrutinizing the data and death certificates, i.e., the CDC or Lyme advocacy organizations, different conclusions have been reached. However, even the broadest interpretation still adds up to a rare percentage of fatalities.
Fortunately, we have treatments to neutralize the disease, and important steps we can take when outdoors to prevent the tick bites that transmit it:
- When you’re home, recheck your entire skin surface for ticks and then shower.
- Put your clothes in the dryer set to high heat to kill any ticks that may be hiding on your outdoor clothes.
Dr. Kallich advises, “always remove your clothing and conduct a full body visual tick check, paying close attention to the crevices, hairy areas, and skin folds where ticks like to hide — a mirror or a close friend with sharp eyes can be a big help with this chore. After that, a warm shower can also help wash ticks off.”
So, before you head out to enjoy nature safely this summer, let’s talk further about Lyme disease with ID Care infectious disease doctor Marsha Kallich, MD.
What Is Lyme Disease?
Lyme is the most common tickborne infectious disease> in the United States. While it’s transmitted through the bite of infected blacklegged ticks (also called deer ticks), the infection itself is caused by a spirochete bacterium, either borrelia burgdorferi (nationwide) or the rarer borrelia mayonii (upper Midwest only). Once in the bloodstream, Lyme spirochetes reproduce and continue to damage the body until countered by effective medication.
Lyme can produce a dizzying array of symptoms, from mild to severe. They can include flu like illness, fever, rash, joint pain or swelling, dizziness, and palpitations, meningitis and sometimes neurocognitive symptoms such as anxiety, depression, vertigo, short-term memory loss, ringing in the ears, light and sound sensitivity, mood swings.
“Lyme can lead to very serious health problems,” said Dr. Kallich, “but it’s something we can handle with a combination of common-sense tick avoidance, modern diagnostic tools, and very effective antibiotic medicines. A bull’s-eye rash rash at the bite location is a common but not universal indicator, and any other Lyme symptom is also a warning to get prompt medical care. It’s the best route to a quick recovery.”
Lyme Disease in New Jersey
The prevalence of Lyme disease in New Jersey is quite high, at 40 cases per 100,000 people, and 2019 saw more than 2,400 cases in the Garden State. Only Pennsylvania and New York exceeded that caseload. Due to abundant tick habitat and a vast whitetail deer population (the tick’s preferred food source), we can expect to be living with Lyme disease in New Jersey for the foreseeable future.
Is Lyme Disease Contagious?
Lyme disease is not contagious as it is not transmitted person-to-person. You can get it only from the bite of a blacklegged tick, also known as a deer tick, and it must remain attached for more than 36 hours to cause an infection. You cannot be directly infected with Lyme by pets or other animals, but they can carry ticks that can infect you, so check your pets for ticks.
Only ticks currently infected with Lyme disease can transmit the disease. They may be active at any time of year, but the most dangerous time is during “tick season,” from April through October. Unfortunately, a recent survey found that up to half of all ticks in the Northeast are infected.
What Should You Do If You Get a Tick Bite?
Any doctor will tell you: the best treatment is prevention. To avoid Lyme disease, avoid tick bites.
But if you are bitten and find a tick attached to your skin, follow these 3 steps:
- Clean the bite location with soap and water or hand sanitizer.
- Call or make a doctor appointment and follow the doctor’s advice.
If you do get infected, the sooner you get antibiotic medication (ideally within 3 days), the better your chances of stopping Lyme disease before it gets a foothold in your body.
Dr. Kallich recommends,“if you develop Lyme symptoms with a tick bite or with no bite, see an infectious disease specialist for an in-person examination and full evaluation, and don’t delay.”
Does Every Tick Bite Cause Lyme Disease?
Lyme can be transmitted only from an infected blacklegged tick attached for at least 36 hours. A bite from an uninfected tick cannot produce the disease.
Even in an endemic area, not all ticks are infected, and the percentage of infected ticks fluctuates yearly and differs by location. So, while not every tick bite can cause infection, every tick bite is a high alert to watch for symptoms of a possible tickborne infection.
Common Signs and Symptoms of Lyme Disease
Lyme can have initial and longer-term effects, but the acute syndrome that develops just after infection is probably the most common: fever, chills, headache, fatigue, muscle and joint pain, swollen lymph nodes, and the bull’s-eye rash otherwise known as erythema chronicum migrans.
Dr. Kallich advised that “the rash is a pretty good sign of Lyme disease, but it doesn’t happen in every patient, so just because you didn’t get the rash doesn’t mean you are free of Lyme disease. However, if you’ve got a swollen joint after developing a bull’s-eye rash, you’ve likely got Lyme disease.”
Lyme Disease Diagnosis
Lyme diagnosis is best if it begins in the clinic of infectious disease experts like ID Care, where a patient history is taken, and physical exam conducted. Is the patient aware of a tick bite? Do they have a bull’s-eye lesion? Do they have a swollen joint? These are red flags for Lyme, and the lab tests that follow will confirm the infection or rule it out. Lyme diagnoses can be complicated by other simultaneous diseases that mimic Lyme.
Dr. Kallich warns that “because of the different pathogens that may be involved, the possibility of multiple infections at the same time, and the other conditions that can mimic Lyme disease, it can sometimes be a confusing diagnosis to make. That’s why if you suspect a Lyme infection, a dedicated infectious disease doctor is your best bet for an accurate assessment and proper treatment.”
How to Test for Lyme Disease
The primary screen for Lyme is an ELISA test (enzyme-linked immunosorbent assay) to detect and measure antibodies in the blood. If that test is negative, you’re disease free. If positive, you may need a second test known as the Western blot. If that is also positive, you have a confirmed case of Lyme disease.
A PCR test (polymerase chain reaction) can detect the presence of Lyme in joint fluid. Some people start with this test, usually due to seeking treatment for a painful, swollen joint. An orthopedist will tap the joint and if it shows a positive PCR, Lyme disease is confirmed.
It’s also important to consider alternative and even multiple diagnoses. For example, a condition that presents like rheumatoid arthritis or lupus could be Lyme. It is possible to have co-infection with other tickborne pathogens like anaplasmosis, ehrlichiosis, and babesiosis. It is possible for a tick carrying more than one type of bacteria to transmit them all with the same bite.
“Usually, especially if a patient is very sick,” said Dr. Kallich, “I’ll test for all potential tickborne diseases at the same time to try to determine what’s really going on.”
A low blood platelet count can indicate infection or non-tickborne autoimmune conditions such as lupus or rheumatoid disease, and these should be investigated with separate testing.
False Negative
It is possible to generate a negative test result and yet still have Lyme. If you get tested early in the course of a Lyme infection, you may have too few bacteria present to trigger a positive result. To account for this, doctors will often start treatment even with before a lab test, if other hallmark symptoms are present.
False Positive
If you’ve had a Lyme infection in the past, you may trigger a positive test result for years afterward, even if you are fully recovered.
To complicate matters, other autoimmune syndromes and spirochetes can trigger an antibody response and produce a positive Lyme test, even when Lyme has never been present. For example, the following diseases have been shown to mimic Lyme disease symptoms:
- Lupus
- Rheumatoid arthritis
- HIV/AIDS
- Syphilis
- Epstein-Barr virus
- H pylori
- Influenza
- Fibromyalgia
With so many illnesses masquerading as Lyme, if a diagnosed patient doesn’t respond to Lyme treatment, further testing may be needed to review the diagnosis and adjust the treatment.
Different Effects of Lyme Disease
A Lyme infection can progress from fairly mild to very severe symptoms, affecting different bodily systems over time. Most people never get beyond the initial acute phase because they get quick treatment and are cured. However, someone with untreated Lyme disease could experience a combination of these effects:
- Lyme arthritis causes serious joint pain in the knee and elsewhere.
- Neurological Lyme disease can appear as Bell’s palsy (facial paralysis), Lyme meningitis, and Lyme radiculoneuropathy, which can present as a pinched nerve or peripheral neuropathy.
- Lyme encephalitis is brain inflammation that can cause chronic symptoms including toxic metabolic encephalopathy and memory problems.
Lyme Disease Treatment
Each patient with Lyme disease should receive a customized treatment plan based on his or her specific case. However, three antibiotics work for the acute stage of Lyme disease: doxycycline, amoxicillin, and cefuroxime. Doxycycline pills are the most used treatment and will usually work within two weeks.
“For Lyme carditis affecting the heart,” said Dr. Kallich, “if it’s mild disease and the electrical block is not too bad, we use doxycycline or amoxicillin. For more severe cases with a longer and more threatening block, we use intravenous ceftriaxone.”
For neurologic disease, also depending on severity, either doxycycline or IV ceftriaxone is a good choice. Lyme arthritis can be more complicated and require longer treatment, which could be doxycycline for a month. If there’s no response or the symptoms persist, doctors may prescribe another course of antibiotics with IV ceftriaxone.
“It’s important to understand that symptoms can persist for a while even with antibiotics,” said Dr. Kallich, “so we tell patients to be patient. Symptoms lasting up to six months is not rare, though most people recover well within that timeframe.
What is ID Care’s Role in Testing, Diagnosing, and Treating Lyme Disease?
ID Care’s role in combatting Lyme disease begins with a thorough patient history, physical examination, and laboratory testing. If a tickborne infection or other illness is detected, we select the right treatment for that specific condition or combination of conditions.
“As infectious disease experts in the hot zone of New Jersey,” said Dr. Kallich, “we’re the specialists you really want to determine if your symptoms are from Lyme disease or something else, ensure proper testing, and to prescribe effective medications for the best outcome.”
For the general public, understanding the risks and ramifications of Lyme is paramount, followed closely by taking appropriate actions to prevent or address a Lyme infection.
“With common-sense precautions you can dramatically reduce your risk of Lyme infection and continue to enjoy the outdoors,” said Dr. Kallich, “but if an infected tick evades your defenses and gives you Lyme, we are ready with a full suite of diagnostic and treatment options to give you the best chance for a complete recovery.”
At ID Care, your health is our priority. If you have symptoms or questions about Lyme, another tickborne illness, or any infectious disease, please call us at 908-281-0610 or visit idcare.com.