This article was medically reviewed by Dr. Rebecca Marsh.
A diabetic foot infection is a complication of diabetes. In the United States, diabetes is a chronic disease that has been on the rise since the 1970s. According to the Centers for Disease Control, more than 37 million people currently have it, about 1 out of every 10 Americans.
The condition is defined by excess glucose (a type of sugar) in the bloodstream, and it puts diabetics at higher risk for many health conditions, including infections of the feet. That’s why it’s important to understand how these infections develop, what risk factors exist, treatment options, and how to prevent getting them in the first place.
For the millions of people affected by diabetes personally or through a loved one, in this blog, ID Care infectious disease specialist Dr. Rebecca Marsh offers critical information on how to properly care for feet, keeping them healthy and free of infection.
What Is Diabetes Mellitus?
Diabetes mellitus, more commonly known as diabetes, is a chronic condition of abnormally high blood sugar. Patients with diabetes are either unable to produce enough of the hormone insulin to metabolize the glucose in their blood, or they are resistant to the insulin they do produce and so cannot metabolize their glucose. This leads to a dangerous excess of glucose in their blood.
“When this happens,” said Dr. Marsh, “it can cause long-term damage to organs, including blood vessels and nerves. Patients can develop problems with their kidneys, eyes, and heart, potentially leading to coronary artery disease. Almost the entire body can be adversely affected by having too much sugar in the bloodstream.”
Diabetes, Foot Infection, and Neuropathy
Among the many long- and short-term health consequences of diabetes, foot infections are an ongoing risk. High levels of glucose in the bloodstream can damage the arteries leading to the feet so that they can no longer supply nerve tissue with adequate nourishment. Over time, this can lead to vascular disease and neuropathy (numbness, tingling, and pain).
If neuropathic numbness worsens, a patient may not notice an initial minor wound for a long time, which allows infection to set in. Sometimes, the numbness can be severe enough that the patient cannot feel the wound even when it is red, swollen, and infected. Worse, blood vessels and nerves are key to fighting off infections, so when they are damaged and can’t function efficiently, any infection has a much easier time spreading.
According to Dr. Marsh, “a blister or cut you don’t know about is one of the biggest risks for trouble with infection. However, patients with diabetes who have not lost sensitivity usually feel a pain in their foot before any other symptom, so they are able to address it promptly.”
She emphasized that “when bacteria set up shop and start developing an overwhelming infection, even in a small area of the foot, it can become bigger and go deeper, leading to deep tissue or bone infections, because the damaged structures can no longer help the healing process.”
Who is Most at Risk of Diabetic Foot Infection?
Those most at risk for diabetic foot infections include patients who:
- Have had diabetes for a long period of time
- Have persistent problems regulating blood sugar
- Have elevated hemoglobin A1C and blood glucose levels
Dr. Marsh advises that “these patients are at higher risk of developing a diabetic foot infection than patients with well-controlled diabetes or those with a new diagnosis. However, anyone who has elevated blood sugar can develop a diabetic foot infection at any time.”
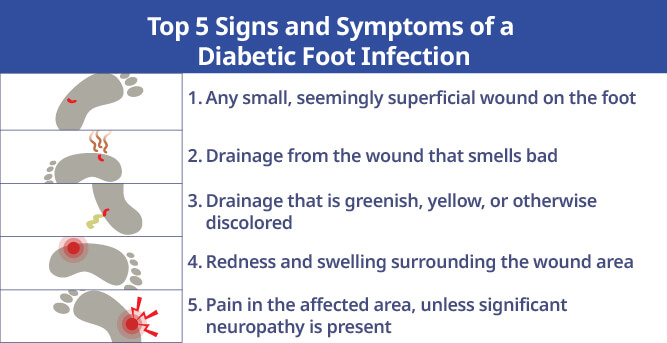
Top 5 Signs and Symptoms of a Diabetic Foot Infection
One of the first signs to watch for is any type of open wound on the foot. This typically includes ulcers, blisters, cuts, and abrasions.
“It could even be a small nick from trimming your toenails,” warns Dr. Marsh, “or a simple blister due to a shoe problem.”
She recommends watching carefully for:
- Any small, seemingly superficial wound on the foot
- Drainage from the wound that smells bad
- Drainage that is greenish, yellow, or otherwise discolored
- Redness and swelling surrounding the wound area
- Pain in the affected area, unless significant neuropathy is present
Consequences of Untreated Diabetic Foot Infection
Left untreated, a diabetic foot infection tends to progress like any cut, abrasion, or blister that becomes infected, potentially leading from the smallest wound to a bone infection, severe tissue damage, or in some cases, loss of the foot.
An infection that cannot be cured even with intensive antibiotic treatment may require amputation once the tissue of the foot is no longer viable. This is a drastic, life-saving measure to prevent the infection from spreading throughout the body and causing death.
Dr. Marsh warns that “a diabetic foot infection can progress from a relatively minor problem to a serious bone infection, then to the amputation of toes, all or part of the foot, or even the leg — people at risk should take this very seriously.”
Is a Diabetic Foot Infection the Same as a Diabetic Foot Ulcer?
No. Diabetic foot ulcers refer to any of the cuts, blisters, or ulcers on your feet that can develop with diabetes. Often early on, those cuts are not infected, even though they could be open and in need of good wound care. If neglected, the problem can worsen.
“Over time, these wounds can get infected,” said Dr. Marsh, “but it is possible to have an ulcer that is not associated with a surrounding infection, so it’s not yet a diabetic foot infection. This is something that ID Care infectious disease doctors see and treat frequently.”
Diabetic Foot Infection Diagnosis
Determining if a patient has a diabetic foot infection involves an exam and clinical diagnosis.
According to Dr. Marsh, “after taking a patient history, we examine their feet for cellulitis or another skin surface infection, as well as signs that the problem goes deeper. If a bone is involved, or if we see anything that looks infected and is draining and foul-smelling with surrounding redness, that’s when we know infection is present.”
To confirm a clinical diagnosis, doctors take a culture of the wound to identify the bacteria. They may also use imaging technology to get a better look at what’s going on under the surface.
“If we’re worried about something we can’t see with the naked eye,” said Dr. Marsh, “we use a CAT scan, MRI, or even an X-ray to help assess the bones and soft tissue in the feet to determine if a worse problem is present, such as an abscess or bone infection.”
Foot Infections Can Create Awareness of Diabetes
Unfortunately, many people have diabetes and don’t know it. They are often diagnosed only when they seek treatment for what they believe is an unrelated foot infection.
“If you have not been diagnosed with diabetes,” advises Dr. Marsh, “and you have a progressive infection in your foot or a skin infection called cellulitis that isn’t healing properly, you could have diabetes that hasn’t yet been diagnosed. See a doctor immediately.”
Diabetic Foot Infection Treatment
When addressing a diabetic foot infection, speed is paramount. The number-one thing to do is to start oral or, depending on intensity of the infection, intravenous antibiotics as soon as possible.
Dr. Marsh said “if someone has had a foot wound for a week or so — perhaps an open ulcer with some surrounding cellulitis that hasn’t spread to the rest of their foot — those are the infections that are much easier to treat and less likely to result in permanent problems like amputation.”
As you might expect, more serious, longer-standing infections are more difficult to treat.
Dr. Marsh warns that, “if you wind up with an abscess or bone infection, you may require surgery to adequately clean out the wound, treat the local surface infection as well as any deeper infection, and remove all the destroyed tissue that cannot be saved.”
The next step is to apply a proper dressing, which may include antimicrobial properties to help further reduce bacteria in the wound. Patients are then closely monitored to make sure their wounds heal appropriately. Those with deeper infections tend to need longer-term solutions to overcome the infection, such as intravenous antibiotics for several weeks, but full recovery is possible even then.
A patient may be hospitalized if their infection is aggressive enough that doctors believe it can’t be treated with oral antibiotics alone. Intravenous antibiotics are more potent, but usually must be administered in a hospital setting, at least initially.
Dr. Marsh advises that patients may also need hospitalization “if they have other signs or symptoms of serious infection such as fever, or if there’s any indication of a severe systemic infection. In those cases, we admit these patients to a hospital.”
The takeaway from Dr. Marsh is very clear: “My biggest concern for these patients is that they get treated quickly and early. In patients with poorly controlled blood sugar, I’ve seen a blister one week become a bone infection the next week.”
In Some Cases, Amputation is Necessary
When patients with diabetic foot infections don’t respond to standard wound care and antibiotics, amputation may be considered. Sometimes the infection can be cured by removing just a small part of the foot, a toe or part of a toe, and then cure any remaining infection with additional antibiotics.
“Unfortunately,” said Dr. Marsh, “sometimes that’s not possible. If the infection is aggressive enough or the patient has diabetic arterial problems, we may need to amputate the forefoot or even the entire foot. In these cases, the only way for it to heal properly is to remove most of the lower leg at the same time. The patient would then need a prosthesis to be able to walk.”
Can a Diabetic Foot Infection Cause Death?
In the same way amputation is a rare but real possibility if treatment is delayed, it is also possible to die from a diabetic foot infection.
For instance, if you have an infection in your foot, you’re diabetic, your blood sugar is not well controlled, and you are not under a doctor’s care, you can wind up with an overwhelming infection called sepsis moving through your bloodstream.
“In those situations,” warns Dr. Marsh, “the worst outcome is possible because it may be too late for doctors to administer treatments that can stop the infection progression leading to death.”
Diabetic Foot Infection Prevention
Fortunately, preventing serious diabetic foot infections is neither complicated nor difficult. Dr. Marsh advises people with diabetes to:
- Take all prescribed diabetes medications: This helps keep your blood sugar controlled so spikes won’t damage vital structures, and infections are less likely to form.
- Inspect and wash your feet every day: Even if your glucose is well controlled, daily foot inspection and cleaning will reveal small or hidden wounds. Pay special attention to areas with thicker, calloused skin.
- Monitor your blood sugar levels: Make sure you’re reaching your blood sugar goal — if not, see your doctor immediately for a more effective treatment plan.
- If you see a wound, go to your doctor or an infectious disease specialist: Do not delay!
- Have a podiatrist examine your feet at least once every year: A podiatrist can also safely clip toenails, minimizing breaks in the skin that can allow bacteria to enter.
- Eliminate any fungal disease from your toenails: Your doctor can help, as fungi can increase the risk of developing a diabetic foot infection.
- Take good care of your feet: Use good-fitting, supportive footwear, and don’t walk around barefoot or in flip-flops. Keeping your feet healthy and protected is the first line of defense against cuts, blisters, abrasions, and the subsequent infections they can cause.
When to See a Doctor
According to the Centers for Disease Control, if you have any of the symptoms listed below, see your primary care physician, a foot doctor, or an infectious disease specialist:
- Leg pain or cramping in your buttocks, thighs, or calves with physical activity
- Numbness and loss of hot/cold sensitivity
- Changing foot shape over time
- Hair loss on toes, feet, and lower legs
- Dry, cracked skin on feet
- Color and temperature change in feet
- Yellowing, thickened toenails
- Fungal infections (such as Athlete’s Foot) between your toes
- Infected corns or ingrown toenails
Dr. Marsh recommends that “if you are at all concerned about any foot wound that isn’t healing normally, see a doctor immediately. The consequences of putting it off are just too serious to risk.”
Which Specialist is Best?
If you suspect a diabetic foot infection, seeing an infectious disease specialist should be first on your to-do list.
Dr. Marsh advises that “many of our ID Care physicians operate in wound care centers, so that’s a perfect place to go because we can treat your wounds while we’re taking care of any underlying infection. Your primary care doctor and your podiatrist are also options to help with a diabetic foot infection.”
What is ID Care’s Role in Caring for People with Diabetic Foot Infections?
“ID Care covers all aspects of diabetic foot infection,” said Dr. Marsh, and “we work in wound care centers where we see a variety of patients – those with wounds with or without diabetes, those with wounds who do have diabetes but aren’t infected, and those with active diabetic infections. We are uniquely qualified to help patients avoid the horrible outcomes that can stem from these infections.”
She added, “we work very closely with podiatrists, vascular surgeons, primary care doctors, and endocrinologists to address all facets of caring for patients with diabetes, including vascular problems and neuropathy, and avoid bad outcomes. If preventing a serious infection is not possible, we also help care for hospitalized patients and those needing surgery or amputations, and manage their IV antibiotics.”
At ID Care, your health is our priority. If you have questions about diabetic foot infections or any infectious disease, please call us at 908-281-0610 or visit idcare.com.