This article was medically approved by Dr. Ajay Mathur.
Accurate information is a top priority when addressing any health concern, especially one as unique as monkeypox, a disease that has generated an abundance of media attention, worry, and speculation. When the diagnosis of the first U.S. case since 2003 hit the news in Spring 2022, most Americans had never heard of monkeypox. When they did, many thought it was a joke or believed incorrectly that it only affected men who have sex with men — the community that was first affected by the current outbreak. As the disease spread, however, facts emerged that everyone can and should understand so we can dispel worry and take the simple steps proven to prevent infection and slow or stop this outbreak.
In this blog, infectious disease specialist Dr. Ajay Mathur provides a complete guide to monkeypox, explaining important details and health effects, as well as how to prevent and treat this illness.
Dr. Mathur’s Top 5 Monkeypox Takeaways:
- Monkeypox is a worldwide disease; it’s no longer restricted to Africa.
- It is not a disease that only affects men who have sex with men; monkeypox can infect anyone.
- Monkeypox transmits primarily through skin-to-skin contact, as well as through respiratory droplets or by contact with textiles used by a person with an infection.
- Monkeypox can be prevented by vaccination.
- Most people will never come across monkeypox — it’s not that common.
“If your doctor isn’t fully familiar with monkeypox, that’s the time to find an infectious disease specialist like the ones at ID Care,” Dr. Mathur added. “Either schedule an appointment directly with us or have your doctor contact us for the right information, the right test, the right treatment, and the right guidance.”
What is Monkeypox?
A pox is a viral disease that produces a rash of painful or itchy pus-filled pimples that can leave pockmarks, or concave scars, upon healing. There are a number of pox viruses, including smallpox, chickenpox, and monkeypox.
“Once monkeypox blisters become fluid-filled,” warns Dr. Mathur, “they can be very painful, especially in sensitive areas such as the anal-rectal area, or in the throat where they prevent people from swallowing food. Normally, these lesions eventually scab over and dissipate.”
The main concern with monkeypox is the pain associated with the rash. It can be located anywhere on the body, and sometimes hospitalization is needed just for pain control. It can be so severe in sensitive areas that people cannot manage the pain at home.
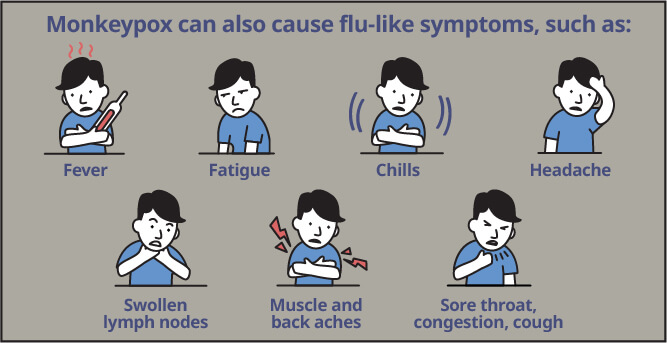
Monkeypox can also cause flu-like symptoms, such as:
- Fever
- Fatigue
- Chills
- Headache
- Swollen lymph nodes
- Muscle and back aches
- Sore throat, congestion, cough
Death is not a common outcome but is possible on rare occasions.
“Typically, those with compromised immune systems are at highest risk for complications, which could include a bloodstream infection called sepsis, or encephalitis, which is swelling of the brain that can lead to death,” Dr. Mathur said. “Fortunately, the overwhelming majority of people who get monkeypox will recover from it.”
How is Monkeypox Transmitted?
The vast majority of monkeypox cases are spread through direct skin-to-skin contact. However, monkeypox is not considered a sexually transmitted disease, because STDs tend to spread through semen or vaginal fluid.
“That’s not necessarily how monkeypox spreads,” advises Dr. Mathur. “It’s mostly from close contact, which could include kissing and cuddling. It could include sexual intercourse, but it doesn’t have to.”
Occasionally, monkeypox can spread through respiratory droplets.
Dr. Mathur advises that, “as with flu or COVID-19, when somebody infected with monkeypox coughs or sneezes, they spread droplets containing the virus into the air. These droplets can infect others, but this route is not common. The vast majority of infections are from direct contact.”
Objects and surfaces can also harbor monkeypox if they’ve contacted the virus either directly or via exhaled droplets, so disinfect surfaces where possible and avoid sharing personal items with someone who has been infected. Things like clothes, towels, and bed linens that have contacted the monkeypox rash can retain and transmit the virus to another person, if that person contacts the item.
How Long Does Monkeypox Last?
After initial infection, a period of incubation takes place which can last between 5 to 12 days. After that, symptoms develop and then typically resolve entirely in about 4 weeks.
Can You Get Monkeypox More than Once?
According to Dr. Mathur, “That’s a question we can’t answer at this point. We’ll need to study people over time to see if subsequent monkeypox infections crop up, or if longstanding antibodies develop to protect against further infections. These are important questions, and I think the answers will come.”
Where Did Monkeypox Come From?
Monkeypox has been a problem for humankind for decades, but until recently, it was mostly contained to Western Africa, where it initially emerged.
The virus was first identified in 1958 after two outbreaks in laboratory research monkeys, though the ultimate source is still not known. There may be a reservoir of monkeypox virus in rodents or non-human primates that continues to infect people in Africa, but in the rest of the world, monkeypox is now clearly a human disease.
Dr. Mathur noted that “most of the minor outbreaks in the last half century have had some relation to West Africa, but the global outbreak we’re seeing now is different.”
The current outbreak hit the United States with a first case in May 2022, and doctors at ID Care were making diagnoses in New Jersey a month later. Cases had previously been seen in the UK, Spain, and other parts of Europe.
“We saw a large peak of cases around mid to late August,” said Dr. Mathur, “approaching 650 cases per day. Now we’re on the downswing, with incidences of monkeypox dropping across our region.”
Currently in the United States, there are more than 25,000 documented cases, with many others likely that have not been documented. According to the CDC, there are 68,000 cases globally, including nearly 30 deaths.
Monkeypox, Chickenpox, and Smallpox
Monkeypox is not necessarily similar to all other pox disease.
“Outside of the name, there’s not much relation between chickenpox and monkeypox, other than the rashes, which can mimic each other at certain stages. But the underlying diseases are not related, and chickenpox is much more common,” said Dr. Mathur.
Smallpox, on the other hand, is more closely related to monkeypox, though it produces a much more severe disease. Smallpox caused significant suffering and death for a large part of human history, but in 1980, it was eradicated from the world after a global vaccine campaign.
“Interestingly,” said Dr. Mather, “the same vaccines work against monkeypox and smallpox due to the close relation of the viruses, so people over 50 who were vaccinated against smallpox as children may have some immunity against monkeypox.”
Who is Most at Risk for Monkeypox?
Monkeypox is not very infectious or common, and until recently has mostly been seen in people from high-risk groups who either travel to or live in Western Africa.
When the virus was localized there, the high-risk groups were children and people with compromised immune systems. These include the very young and very old, people with immune conditions such as HIV/AIDS, and those on immune-suppressing drugs for conditions such as organ transplants.
In the worldwide outbreak of 2022, however, up to 98% of the cases in a study published in August 2022 were shown to have occurred in men who have sex with men. This is thought to be largely a coincidence — that is, the virus infected a person who then attended one or more large gatherings that included men who have sex with men, which gained it access to that population, where it spread by skin-to-skin contact.
This current outbreak has been linked to large dance parties that took place in the gay community in Europe. Even though they weren’t explicitly sexual, these events happened during warm-weather months and involved people wearing light clothing and engaging in lots of socializing, close dancing, and skin-to-skin contact, so the virus was able to spread among that population.
“The important thing to remember,” warns Dr. Mathur, “is that monkeypox can affect anybody, including children, pregnant people, and other immune-compromised people. We’re starting to see a downward trend in infections among gay men, and a rise in cases in other populations, such as heterosexual males and females, as well as a few cases in children.”
Where is Monkeypox Most Likely to be Transmitted?
The more time you spend in contact with someone who has monkeypox, whether they know they have it or not, the more likely you are to get infected. Avoid settings where such contact is likely.
Dr. Mather warns that “the most dangerous situation would be where you have multiple sexual partners that you don’t know well, regardless of their gender or physical attributes. That maximizes the likelihood that you’ll come in close contact with a person who has the infection without knowing it.”
Hospitals and other types of healthcare facilities can also raise the risk of transmission, especially for healthcare workers, if infection prevention is not executed properly. Facilities that want to implement or maintain the latest, best infection control protocols for monkeypox or any disease should consult with infectious disease specialists like those at ID Care.
Should Parents Worry About Monkeypox in Schools?
Dr. Mather is optimistic that, “as this wave of infection continues to slow down, the risk to schoolchildren seems very low. Most children are not in high-risk categories, and the type of skin-to-skin contact that transmission usually requires is not taking place in schools, nor is the sharing of clothes or linens. Most parents should feel confident that monkeypox transmission in schools is very unlikely at this time.”
How is Monkeypox Diagnosed?
A patient history and physical exam can help narrow down a diagnosis, but a PCR (polymerase chain reaction) test can definitively diagnose a monkeypox infection. This test functions much like the PCR test for COVID-19, with a swab taken of the infected area and sent to a laboratory. The presence or absence of viral proteins will be determined there.
How is Monkeypox Treated?
In general, for most people who are otherwise healthy and don’t have any major immune suppression issues, this infection will come and go without any specific treatment in about 4 weeks.
For the subset of people at higher risk for complications, a medication called TPOXX is available to treat monkeypox. It is a component of the treatment for smallpox, but can be effective on monkeypox as well, and is the standard of care right now in the United States.
TPOXX is available in an IV formulation for patients who can’t swallow pills, but most people take their TPOXX in pill form. Treatment usually takes from 1 to 2-weeks to fully clear a monkeypox infection.
“Beyond vaccination and TPOXX,” advised Dr. Mathur, “treatment is focused on pain control. Some people require a lidocaine patch to manage it, and others may need oral pain medications.”
How Can We Prevent Monkeypox Infection?
Preventing monkeypox infection is straightforward and usually easy to implement:
- Pay attention to your health and that of your partner(s) and people in your household, especially to any unexplained rash.
- If you suspect a monkeypox infection, isolate the person from others until the infection status can be determined.
- Do not have sexual relations or close physical contact with the person who is possibly infected.
- Do not share clothes, towels, bed linens, or similar items with the isolated patient.
- As soon as reasonably possible, the potentially infected person should see a doctor, ideally an infectious disease specialist like those at ID Care.
Is There a Monkeypox Vaccine?
The main monkeypox vaccine available now is called Jynneos, and it is also approved for smallpox. It’s a two-shot series, with about a month between each injection. It is intended only for the highest-risk patients, or for people thought to have been exposed to the monkeypox virus. A less-commonly used vaccine called ACAM2000 is also an option. It was originally licensed to prevent smallpox, but is now authorized for monkeypox as well.
According to Dr. Mathur, “Getting vaccinated within 3 or 4 days of exposure to monkeypox can stave off the infection or at least make it much milder, so it’s worth trying in those cases.”
In late September 2022, the CDC released information from vaccine studies indicating that those who have not received any vaccine are 14 times more likely to get infected with monkeypox than people who have been fully vaccinated. Even one injection, or half a full dose, provides some protection, although the full dose works much better and is recommended.
When Should You See a Doctor?
While monkeypox can have serious consequences for certain high-risk people, it is not a life-threatening emergency for the great majority of people. Nevertheless, seeking treatment quickly is still important.
Dr. Mathur encourages anyone who has a rash or suspects monkeypox to see a healthcare professional quickly, primarily to obtain testing to determine if the condition is actually monkeypox or another viral illness with a similar looking rash, such as chickenpox or shingles.
“If we wait until the lesions go away, we don’t get the full answer, and we can worsen viral outbreaks by making incorrect assumptions,” Dr. Mathur said. “Getting a PCR test and having it properly interpreted is super important to helping stop or slow any outbreak.”
What is ID Care’s Role in Diagnosing and Treating Monkeypox?
ID Care is a leader in infectious disease treatment in New Jersey, so when it was clear the monkeypox outbreak would reach our shores, ID Care doctors began obtaining PCR tests so that they would be able to check patients in their offices. Their expertise in infectious disease control and treatment makes them uniquely qualified to address this outbreak.
“We are the doctors who can recognize the rash, differentiate it from other infections, and do the in-office testing and interpretation without the need for a visit to the ER or to an urgent care facility,” Dr. Mathur noted.
ID Care also serves as a resource for higher-risk patients, finding available vaccine doses across New Jersey and guiding people on vaccination, TPOXX and other treatments, and preventative behavior modification. “That’s really where ID Care doctors step up and provide that next level of care for our patients,” Dr. Mathur emphasized.
At ID Care, your health is our priority. If you have questions about monkeypox or any infectious disease, please call us at 908-281-0610 or visit idcare.com.