This article has been medically review by Dr. Syed Husain.
Most people don’t anticipate that seeking care in a hospital or non-hospital healthcare facility could end up making them sicker. Yet, the Centers for Disease Control and Prevention (CDC) reports that 1 in 31 hospital patients acquire an infection that has the potential to cause serious illness or even death while receiving care for another condition. Fortunately, healthcare facilities and patients can use preventive methods that have been shown to reduce the incidence of certain healthcare-associated infections by up to 70%.
In this blog about “healthcare-associated infections: causes and prevention,” Dr. Syed Husain of ID Care explains what HAIs are, where and how they are contracted, and what patients and medical teams can do to prevent them. “All of the infectious disease specialists in our practice take this issue extraordinarily seriously,” Dr. Husain said. “We are committed to using every approach in our toolbox to prevent HAIs, both by supporting facilities in complying with precautionary guidelines and by educating patients.”
But how do patients come out of healthcare settings with infections they didn’t have when they went in? HAIs can be transmitted when germs get into surgical wounds or enter patients’ systems through invasive medical equipment such as catheters or central lines. The overuse of antibiotics can also lead to healthcare-associated infections.
Infections are considered HAIs if they develop as follows:
- in a healthcare facility when a person was admitted for unrelated reasons
- 48 hours or more post admission
- within 3 days post discharge
- within 30 days post medical procedure
Using accepted practices to prevent HAIs is the responsibility of:
- Healthcare facilities, which must institute and follow infection prevention and control plans, often with the help of infectious disease doctors like those at ID Care.
- Government agencies, which monitor and report the outcomes of these plans and infection rates.
- Patients, who must avoid touching their surgical wounds or invasive medical devices associated with a procedure or treatment, such as a catheter or ventilator, especially if they are immunocompromised; they should also tell their medical teams about any symptoms that might signal the presence of an infection.
All these measures are crucial because patient health outcomes and the reputations of healthcare facilities depend on them.
What is a Healthcare-Associated Infection?
An HAI, often referred to in clinical settings as a “nosocomial” infection, develops while a patient is being cared for on an inpatient or outpatient basis in a healthcare facility, and is the result of bacteria, a virus, or fungus entering the body. These germs can enter through a wound, invasive medical equipment such as a catheter or ventilator, or the lungs. The result is that a patient leaves the healthcare facility with an illness that he or she did not have upon admission.
Where Can People Contract Healthcare-Associated Infections?
For many years, HAIs were known as “hospital-acquired infections,” but that term has been updated to reflect the fact that patients can contract healthcare-associated infections in any setting where they receive care:
- hospitals
- ambulatory surgery centers
- rehabilitation facilities
- wound care centers
- nursing homes
- long-term care facilities
- dialysis centers
- community clinics or doctors’ offices
- home care settings
What Are Common Types of HAIs?
Healthcare-associated infections fall into several common types based on the medical procedures and devices that have transmitted pathogens to a patient.
- Surgical site infections, which can arise at the spot where medical devices entered the body during surgical procedures such as coronary artery bypass, appendectomy, cholecystectomy, or the removal of an abscess or mass.
- Catheter-associated urinary tract infections (CAUTIs) can occur when germs are present on catheters that are used to monitor or facilitate a patient’s urine output.
- Central line-associated bloodstream infections can crop up when pathogens are present on lines used to facilitate and monitor a patient’s intake and output of fluids and/or to administer medications.
- Ventilator-associated pneumonia or other infections can arise when ventilators are used to assist patients with breathing.
- Clostridium difficile, a multidrug-resistant infection of the large intestine that causes diarrhea and can be fatal, can sometimes arise when patients are treated with antibiotics. Even though antibiotics are essential to the treatment of numerous infections, including some HAIs, certain types called broad-spectrum antibiotics are more likely to result in C. difficile infections. Fluoroquinolones are a primary example of this category of antibiotics.
“When patients come in with complicated infections, they may need broad-spectrum antibiotics. While receiving these antibiotics, they are at risk of developing Clostridium difficile colitis, a type of infection that causes diarrhea, because the medication may eliminate what we consider ‘good’ bacteria in the intestines along with the bad,” Dr. Husain said. “These kinds of infections are particularly dangerous because they have become resistant to certain antibiotics, and they are more commonly to blame for HAIs these days than they were in the past. That’s why such pathogens must be treated with speed, vigilance, and expertise by infectious disease doctors like those at ID Care.”
What Germs Cause Healthcare-Associated Infections?
Multiple types of pathogens can cause HAIs, and they fall within three categories. From the most to the least common, these categories are bacteria, fungi, and viruses. Within each category, there are germs that can cause more than one of the common types of HAIs.
Pathogens that Cause HAIs Include:
- Bacteria such as Staphylococcus aureus (MRSA), Clostridium difficile, Enterococci, Acinetobacter, Pseudomonas aeruginosa, E. coli, and Enterobacterales
- Fungi such as Candida albicans and Aspergillus spp.
- Viruses such as hepatitis, HIV, respiratory syncytial virus (RSV), and COVID-19
Who is Most at Risk for a Healthcare-Associated Infection?
Determining a patient’s risk of contracting an HAI comes down to a simple equation: the longer someone is treated, the greater his or her risk is of getting one of these infectious diseases.
“Any patient who is treated for a long time using a catheter, a ventilator, central lines, or antibiotics is at increased risk,” Dr. Husain said. “This is because anything that lowers someone’s immunity while potentially increasing the presence and duration of foreign bodies during their care can predispose them to a healthcare-associated infection.”
In addition, health conditions or treatments that cause immunosuppression can contribute to a patient’s likelihood of contracting an HAI, including:
- Older age
- HIV/AIDS
- Cancer
- Diabetes
- Rheumatoid arthritis
- Implanted medical devices such as pacemakers or artificial joints
What are Healthcare Facilities Doing to Prevent HAIs?
Healthcare facilities of all kinds are committed to keeping their rates of HAIs as low as possible by creating guidelines and training staff members to follow them. These guidelines are set by each facility’s infection control and prevention department according to regulations mandated by law. Then, a multi-specialty team works together to ensure timely and accurate execution and oversight.
Hospitals, nursing homes, and other healthcare facilities frequently hire ID Care doctors to help formulate and supervise these infection control plans, which must include processes for recording HAIs in a database and reporting them to local, state, and federal regulatory authorities. This is done not just to identify the problem, but to help ensure that accepted practices and procedures, such as tracking down the source of the infection, are used to make sure the issue does not recur. At certain intervals, governmental agencies such as the Joint Commission on Hospital Accreditation, dedicated to quality care and patient safety, visit healthcare facilities to ensure that they are following good infection control practices and to gather information for reporting.
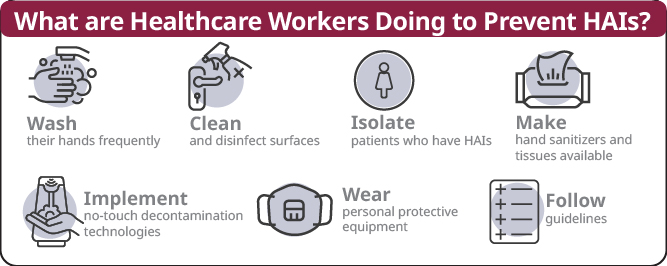
Dr. Husain, who serves as Chair of Infection Control at St. Francis Medical Center in Trenton, N.J., and plays a leadership role in drafting such plans at other top institutions, always makes sure that guidelines direct healthcare workers to:
- Wash their hands frequently
- Clean and disinfect the surfaces in patient rooms
- Isolate patients who have HAIs
- Make hand sanitizers and tissues available
- Implement automated no-touch decontamination technologies
- Wear personal protective equipment (PPE), such as gowns, gloves, masks, and eye coverings
- Follow guidelines for dealing with blood and contaminated items
Does Restricting Antibiotic Use Help Prevent HAIs?
Any plan for preventing HAIs should call for careful consideration when it comes to the prescription of antibiotics, because the overuse and misuse of these drugs can contribute to specific types of bacteria becoming resistant to treatment. As a result, antibiotics must be prescribed only for conditions that will respond to them — for example, infections but not viruses — in the right dose and for the right duration.
“A coordinated program of thoughtful, conservative management of antibiotics is one of the greatest responsibilities of infectious disease specialists like myself and my colleagues at ID Care,” Dr. Husain said. “We refer to this as antibiotic stewardship, and it helps immensely in preventing healthcare-associated infections because the unnecessary use of these medications can predispose patients to dangerous, drug-resistant bacteria. Experts in this area know that it’s essential to disperse antibiotics intelligently and only when they are truly needed.”
Does COVID-19 Make it Harder to Prevent HAIs?
Long before the emergence of COVID-19, healthcare facilities were following plans designed to protect patients and workers from HAIs. But the spread of the virus has created a need for stricter rules and greater adherence to them — particularly because COVID-19 is considered an HAI when it is contracted in healthcare settings.
Enhanced COVID-19 protective measures include:
- adding eye shields to PPE because COVID-19 can spread into mucous membranes such as the eyes
- limiting the number of visitors to patients who have the virus
- doing extra cleaning within facilities
- restricting movement through the building by staff members who have treated affected patients.
“The most important aspect of enhanced infection prevention in these unusual times has been education, which has been ramped up as we’ve worked through pandemic conditions,” Dr. Husain said.
How Can Patients Avoid Healthcare-Associated Infections?
Patients who understand the causes of healthcare-associated infections can also learn how to avoid them, protecting themselves by following some simple rules:
- Do not touch wounds or medical equipment. “If there are lines or catheters in place, patients should not touch or take them out, but instead leave that to the nursing staff or physicians,” Dr. Husain said. “Our team at ID Care has observed that sometimes an inserted catheter, line, or surgical wound cannot be appropriately managed because the patient has manipulated it, and that raises the risk that the patient might develop an HAI.”
- Ask questions. Patients should always feel comfortable asking nurses and doctors what is being done to protect them against infections, whether a medical device such as a catheter remains necessary, and whether recommended antibiotics are the appropriate choice and for what duration, or if they are even needed at all.
- Watch for symptoms. Patients should immediately report fever, diarrhea, or skin redness or puffiness, which could signal infection.
Patients who are specifically worried about contracting COVID-19 in a healthcare setting should consider postponing elective procedures only when caseloads are high. When procedures are urgent, patients should move forward with confidence that their facilities are working to prevent HAIs through their infection prevention and control plans.
Why is it Crucial to Prevent Healthcare-Associated Infections?
No discussion of healthcare-associated diseases, including causes and prevention, would be complete without some thoughts about why ID Care considers it so important to protect patients and healthcare workers from these dangerous infections.
Of course, the most obvious reason to work hard to prevent HAIs is to help ensure safe, quality care and good health outcomes for patients who receive treatment in healthcare facilities. But healthcare organizations also face other concerns.
One involves the costs generated when time, equipment, and medication are devoted to treating infections that could have been prevented. In fact, high infection rates can lead to facilities being penalized by the Centers for Medicare & Medicaid Services, a government authority responsible for tracking HAI rates, through a reduction in reimbursements for patient care.
The reputations of healthcare facilities also depend on good infection prevention and control, since HAIs are reported publicly and can thus factor into patients’ decisions about where to seek treatment and whether they would recommend a facility to friends or family.
What is ID Care’s Role in Preventing Healthcare-Associated Infections?
“ID Care is heavily involved in guiding New Jersey’s healthcare organizations in establishing and implementing their infection prevention and control practices, and this expert advice is probably the most significant way we are able to help prevent the development of HAIs in facilities throughout the state,” Dr. Husain said.
Of course, the 50 infectious disease doctors who compose the ID Care team are just as prepared to care for patients who do develop healthcare-associated infections. “Our mission is to provide them with appropriate management and treatment so that they get better, while also consulting with their treating facilities to prevent these infections from happening again in the future,” he said.
ID Care provides comprehensive care for all infectious diseases in its 10 outpatient locations as well as in healthcare facilities throughout New Jersey. To consult with an infectious disease expert today or enhance your facility’s infection control policies and plans, call 908-281-0610 or visit idcare.com.